During the COVID-19 pandemic, our clinical nutrition team has been tasked with preparing meals that will help COVID-19 patients heal.
They’ve also worked throughout the health care system to provide patients with a healthy diet and a sense of normal.
Through it all, they’ve risen to the challenge of providing not only nutritional support, but emotional support as well.
Food is fuel, whether you’re at work, exercising or, like patients at Regional One Health, battling illness or injury. During the pandemic, our clinical nutrition team is rising to the challenge of providing meals that help patients heal and address diverse, rapidly evolving symptoms.
“They’re here every day, on weekends, on holidays, caring for patients,” said Clinical Nutrition Manager Jacqueline Daughtry, RDN, LDN. “They’ve shown incredible dedication and teamwork. I’m extremely proud of the team and I’m honored to be their leader.”
The virus impacts clinical dietitians throughout the hospital.
In trauma and subacute, dietitians are accustomed to helping critically ill patients – but COVID-19 is a new challenge. Where they used to rely on experience and precedent to anticipate and support a patient’s recovery, coronavirus causes frequent ups and downs that require quick adjustments.
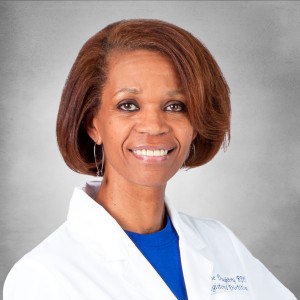
Clinical Nutrition Manager Jacqueline Daughtry is proud of her team’s work during the pandemic: “They have shown incredible dedication and teamwork.”
“These patients can change so quickly. They can be relatively stable one minute, and then 30 minutes later they’re being transferred to intensive care,” Sarah Heyrman, RD, LDN, said.
“It isn’t just respiratory – it can affect multiple organs and systems,” Paige Crawford, MSRD, LDN, added. “Patients’ status can change every day. If we don’t provide the right nutrition for their status, it can be the difference in whether they recover.”
To address those issues, Katara Jackson, MPPD, RDN, LDN, rounds with the doctors and nurses in the unit. “A lot of patients are struggling with comorbidities like obesity and kidney and liver issues,” she said. “We monitor their lab work closely to watch for changes.”
“By being right there with the medical team, we can create interventions immediately with physicians’ input,” Daughtry explained. “With COVID-19, different organs fail unexpectedly and the presentation changes rapidly, so we’re doing a lot more interventions.”
The challenges also reach units that aren’t directly caring for COVID-19 patients.
In antepartum, Penelope Denny, RDN, LDN, is both dietitian and cheerleader for expectant moms: “Because of the visitor guidelines, these moms are in the hospital for weeks or months all by themselves. They can get depressed from the isolation, and their food intake goes down.”
Denny asks about favorite meals, provides healthy comfort foods and encourages patients by reminding them eating well helps their baby grow. She also monitors their weights to assess trends.

The clinical nutrition team has worked hard to provide dietary and emotional support to help patients heal.
In the NICU, families are dealing with the dual challenges of a pandemic and having a newborn in need of critical care. NICU dietician Adriann Skeen, MS, RDN, LDN said her day-to-day work of providing tiny premature infants the nutrients they need to grow and get stronger has not changed, so she focuses on providing a healthy diet for the babies and support for their parents.
Outpatient nutritionists, meanwhile, focus both on ensuring patients can safely receive services and promoting good nutrition during a time of stress.
Jenifer Chang MA, RDN, LDN spearheads Medical Nutritional Therapy for patients with diabetes, obesity and kidney disease, while Emily Faquin RDN, LDN works with HIV-positive patients, including expectant moms.
Chang provides group classes and face-to-face consultations, so she reassures patients Regional One Health is making it safe to seek care. She’s also finding alternative ways to reach out, even adding a class at the East Campus to help more patients attend.
“If patients aren’t comfortable coming in, we talk by phone, or I email or mail them nutrition education information,” she said. “For the MNT classes, we’re trying to be flexible and listen to what they need.”
Regional One Health will soon be offering telehealth for all MNT, and it is currently available for the nationally accredited Diabetes Self-Management Education program.
Faquin noted pandemic-related stress can make medical conditions worse, so it’s important to keep reaching out. “Stress affects your appetite, and a lot of people end up undereating or overeating,” she said. “That affects your overall health, so it’s kind of a domino effect.”

“If COVID-19 has taught us anything, it’s that we’re your educator, your cheerleader, your support team,” dietician Paige Crawford said. “These are real people and real families going through this, and we want to be the life raft going out to them.”
“We encourage them to eat healthy, whole foods and take vitamins,” Chang said. “We talk a lot about physical activity and exercises they can do at home, like taking a walk or gardening.”
Faquin also connects patients with support services. “One of the most important things you can do is listen and be sympathetic. If a patient tells me they’re stressed or depressed, I work with their case manager to get counseling. If they’re struggling with food insecurity, I call around and find places they can get food.”
Addressing emotional and social needs is a common thread for the nutrition team. “Eating is a normal process, but when people are traumatized, it can be hard,” Crawford said. “We can give them normalcy if we’re compassionate and consider everything going on in their lives.”
They can also give them the building blocks to recovery, and Heyrman doesn’t miss a chance to remind patients of that. “I tell them, ‘Just like a car needs fuel, your body needs nutrition to keep going.’ I let them know that if they don’t eat, they aren’t losing fat, they’re losing muscle, and that can cause them to become weaker and have a snowball effect.”
Fortunately, they’ve found that a friendly face and a healthy, appealing meal can remind patients of the normal parts of life they’re fighting to reclaim.
“If COVID-19 has taught us anything, it’s that we’re your educator, your cheerleader, your support team,” Crawford said. “These are real people and real families going through this, and we want to be the life raft going out to them.”

